Obsessive-compulsive disorder (OCD) is not classified as an anxiety disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). While OCD often involves intense anxiety and commonly co-occurs with anxiety disorders, it is now placed in its own category: Obsessive-Compulsive and Related Disorders.
About 1.2% of U.S. adults experience OCD in a given year, and 2.3% will experience it at some point in their lives. Globally, OCD affects an estimated 1–3% of the population. These numbers underscore the importance of accurate classification and treatment.
What is OCD?
Obsessive-compulsive disorder (OCD) is a mental health condition marked by two core symptoms:
- Obsessions: Unwanted, intrusive thoughts, images, urges, feelings, or sensations that cause significant anxiety or distress.
- Compulsions: Repetitive behaviors or mental rituals performed to reduce the anxiety triggered by obsessions or to prevent a feared event.
This obsession-compulsion cycle can be time-consuming, emotionally draining, and disruptive to daily life.
Why OCD was reclassified
While OCD certainly involves anxiety, it is not classified as an anxiety disorder in the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5). In 2013, OCD was placed into its own category: Obsessive-Compulsive and Related Disorders, which also includes:
- Body dysmorphic disorder (BDD)
- Hoarding disorder
- Trichotillomania (hair-pulling disorder)
- Excoriation (skin-picking disorder)
This reclassification reflects the unique features of OCD, especially the repetitive, ritualistic behaviors and the specific nature of intrusive thoughts.
“Every person with OCD experiences anxiety,” says Tracie Ibrahim, LMFT, CST, Chief Compliance Officer at NOCD. “No one with OCD has ever escaped the feeling of anxiety—that’s the whole problem—that you feel so anxious that you engage in compulsions to try to get rid of the discomfort of the anxiety.”
How are OCD and anxiety disorders related?
Although OCD is not classified as an anxiety disorder, the two are closely linked.
- Anxiety is a core feature of OCD: Obsessions (intrusive, distressing thoughts) trigger anxiety, and compulsions are performed to temporarily relieve that anxiety.
- High comorbidity rates: Research shows that many people with OCD also meet criteria for at least one anxiety disorder. For example, a study of children and adolescents found that nearly half also had another anxiety disorder.
- Shared symptoms: Excessive worry, restlessness, and physical tension may appear in both OCD and generalized anxiety disorder (GAD).
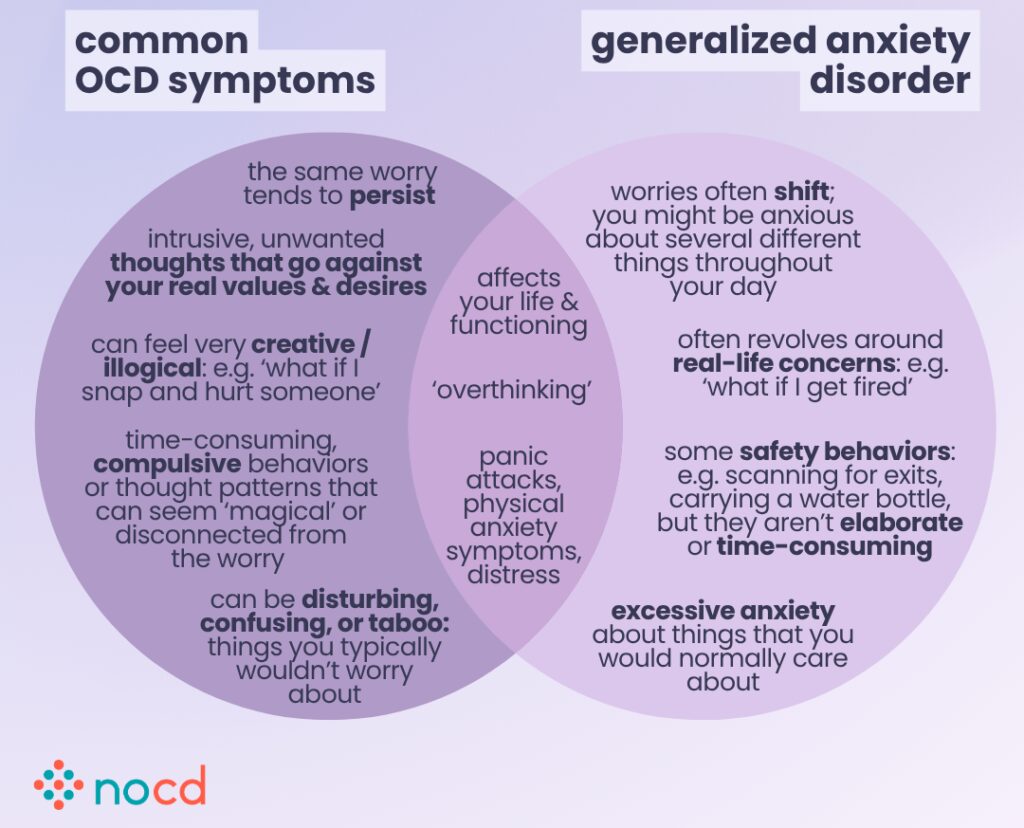
The key distinction is that in OCD, anxiety is driven by intrusive thoughts and maintained by compulsive behaviors, which is different from the broader worry patterns seen in generalized anxiety disorder.
Key differences: OCD vs. anxiety disorders
Here’s a closer look at how OCD differs from other anxiety disorders like generalized anxiety disorder (GAD), panic disorder, or social anxiety:
1. OCD follows a specific pattern
OCD typically follows a structured cycle: intrusive thought (obsession) → Intense anxiety → compulsion to neutralize the fear → temporary relief.
In contrast, anxiety disorders often involve persistent worry or fear without ritualistic behaviors.
2. Compulsions are central to OCD
People with OCD perform rituals or mental acts (e.g., checking, counting, reassurance-seeking) in response to their obsessions.
In anxiety disorders, behaviors are generally reactive, not ritualistic.
“There’s only one thing that makes OCD and anxiety different, and that’s obsessions and compulsions,” says Ibrahim.
3. OCD themes are more specific and repetitive
OCD often fixates on themes such as:
- Contamination
- Harm
- Morality
- Order or symmetry
While anxiety disorders may involve similar fears, they usually focus on real-life scenarios and are less repetitive or irrational in nature.
Comparison chart: OCD vs. anxiety disorders
Below is a quick comparison chart to help clarify:
| OCD | Anxiety disorders |
| Involves unwanted, intrusive thoughts (obsessions) | Involve excessive worry, fear, or dread about future events or social situations |
| Leads to compulsive behaviors or mental rituals to neutralize anxiety | Does not involve physical or mental compulsions |
| Follows a repetitive cycle → obsession → anxiety → compulsion → temporary relief | Worries are often tied to real-life situations |
| Often centers around specific themes, such as contamination, morality, or harm | Anxiety is usually triggered by specific situations, not by intrusive thoughts |
Can you have OCD and an anxiety disorder?
Yes. It’s very common to have both OCD and an anxiety disorder. Research suggests that around one-third of people with OCD also meet criteria for a co-occurring anxiety condition, such as:
- Generalized anxiety disorder (GAD)
- Social anxiety disorder (SAD)
- Specific phobias
Comorbidity can make symptoms more intense and harder to treat, as each condition can reinforce the other.
Treatment for OCD and anxiety disorders
Effective treatment is available—and often tailored to the diagnosis.
OCD Treatment: ERP therapy
- The most effective treatment for OCD is exposure and response prevention (ERP) therapy, a type of cognitive behavioral therapy (CBT). General CBT alone may not be effective for OCD and can even worsen symptoms if not properly tailored.
- ERP helps individuals face anxiety-provoking thoughts without engaging in compulsions.
“ERP helps people tolerate discomfort and teaches them that they don’t need to perform compulsions to feel safe,” says Ibrahim.
Studies show that ERP therapy is highly effective, with 80% of people with OCD experiencing a significant reduction in their symptoms.
Other approaches that may help include:
- Medication (typically SSRIs)
- Mindfulness-based strategies
- Acceptance and commitment therapy (ACT)
These are typically done in combination with ERP therapy, depending on the individual’s needs.
Severe or treatment-resistant OCD may benefit from the following therapies:
- Intensive outpatient programs (IOPs)
- Partial hospital programs (PHPs)
- Residential treatment centers (RTCs)
- Transcranial magnetic stimulation (TMS)
- Deep brain stimulation (DBS)
- Gamma knife radiosurgery (GKRS)
Find the right OCD therapist for you
All our therapists are licensed and trained in exposure and response prevention therapy (ERP), the gold standard treatment for OCD.
Anxiety disorder treatment
- Standard CBT and sometimes medication (like SSRIs) are commonly used.
- ERP therapy can also be effective for treating anxiety disorders.
Bottom line
Although OCD and anxiety disorders share similar symptoms, they are distinct mental health conditions. The key difference lies in the presence of obsessions and compulsions, which are unique to OCD.
Understanding this distinction is crucial for getting the right diagnosis and receiving evidence-based treatment.
Key takeaways
- OCD is not currently classified as an anxiety disorder, despite anxiety being a core feature.
- The defining traits of OCD are intrusive thoughts (obsessions) and compulsive behaviors.
- Anxiety disorders often involve worry and fear, but not ritualistic compulsions.
- Many people experience both OCD and an anxiety disorder, and both are treatable.
- Exposure and Response Prevention (ERP) therapy is a highly effective treatment for OCD and anxiety disorders.
